Home / Diseases & Conditions / Obstructed Defaecation
Obstructed Defaecation
Obstructed defaecation (OD) is a condition where a person has difficulty emptying their bowel despite feeling the urge to pass a stool. It is a form of chronic constipation caused by problems with the mechanics of bowel emptying rather than slow bowel movement.
Obstructed defaecation is more common in women, particularly after childbirth, and can become more noticeable with age.
It is often associated with pelvic floor dysfunction or structural issues within the rectum or pelvic area.
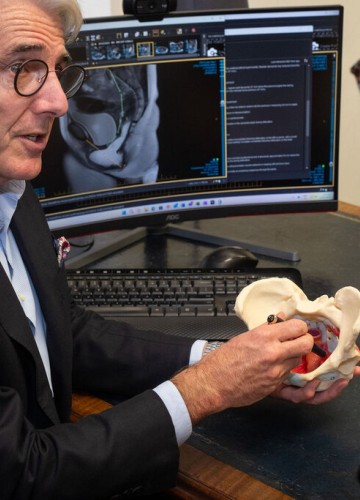
Diagnosis is usually made through a detailed assessment of symptoms, physical examination, and specialised tests such as a defaecating proctogram, anorectal physiology or endoanal ultrasound.

Symptoms of Obstructed Defaecation
Symptoms of obstructed defaecation can vary but commonly include:
A sensation of incomplete emptying after passing a stool
Needing to strain excessively to open the bowels
A feeling of blockage or obstruction during defaecation
The need to use fingers to help empty the bowel
Prolonged time spent trying to pass a bowel motion
Some people may also notice symptoms of pelvic organ prolapse or urinary symptoms.
Causes of Obstructed Defaecation
Treatment of Obstructed Defaecation
Treatment for obstructed defaecation is highly individualised and aims to improve bowel emptying and quality of life. It may involve conservative measures, pelvic floor physiotherapy, and, in some cases, surgery.
Managing obstructed defaecation often involves working closely with a team that may include a colorectal surgeon, pelvic floor physiotherapist, and dietitian.
Although OD can be distressing and impact daily life, many people improve with tailored treatment. Identifying the underlying cause is key to successful management.
If you are experiencing ongoing difficulty with bowel emptying, speak to a colorectal surgeon.
Conservative Management
Dietary changes: Increasing fluid and dietary fibre intake may help.
Stool softeners or laxatives: May be used to ease passage of stool.
Bowel retraining: Establishing a regular toilet routine.
Pelvic Floor Physiotherapy can help Pelvic floor exercises may help improve muscle tone and function and correct muscle coordination when passing a bowel motion.
Surgery
Surgery is considered if conservative and physiotherapy approaches are not effective, and if a clear structural abnormality is contributing to symptoms.



