Home / Diseases & Conditions / Rectal Prolapse
Rectal Prolapse
Rectal prolapse is part of the rectum, the lowest part of the large bowel, protruding out through the anus. It often needs surgery to fix it, but sometimes non-surgical treatment can help with the symptoms.
What are the symptoms of rectal prolapse?
Symptoms of rectal prolapse can include:
A pink fleshy lump protruding from the anus, especially when having a bowel motion. It may go back by itself or need to be pushed back inside. Sometimes it won’t go back.
Faecal Leakage which may be anything from some mucus causing moistness around the anus or staining the underwear to complete loss of bowel control, faecal incontinence.
Bleeding from the anus, often pink and watery.
Feeling that your rectum isn’t completely empty after a bowel motion
Treatment of Rectal Prolapse
A thorough assessment is essential to ensure the most effective treatment for rectal prolapse.
Rectal prolapse is often linked to problems affecting other pelvic organs and structures.
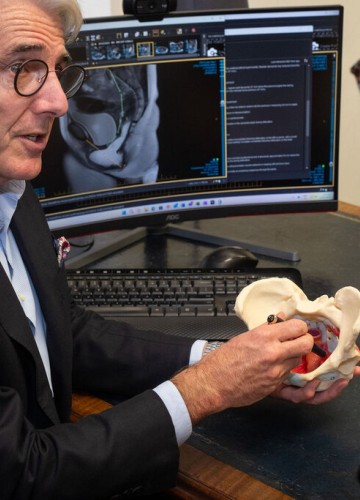
Understanding the full extent of the rectal prolapse, any associated conditions such as haemorrhoids or inflammation, the state of nearby organs such as uterus, vagina, bladder and prostate, and the function of the pelvic floor muscles and anal sphincter muscles is crucial for planning treatment.
To build a complete picture of your condition, your colorectal surgeon may recommend investigations including anorectal physiology, endoanal ultrasound, and dynamic pelvic MRI.
There are a number of surgical procedures that can fix rectal prolapse.
It is important talk to your surgeon to find the best option for you.
Procedures used to manage rectal prolapse include Delorme's procedure, Altemeier procedure, and ventral mesh rectopexy.
Discussing rectal prolapse with a colorectal surgeon specialising in pelvic floor disorders can help you get a personalised management plan to improve your symptoms and quality of life
Intus colorectal surgeons are experienced in the treatment of rectal prolapse and will support you through assessment and treatment.
Stool Softeners
To help make soft formed stools that are easier to pass with less need to strain.
Suppositories
To help with bowel movements and ease symptoms.
Dietary Changes
Eating more fibre and drinking plenty of fluids can help prevent constipation.
Medications
To prevent diarrhoea where that is aggravating the prolapse.
Pelvic Floor Physiotherapy
To strengthen pelvic floor muscles, reduce straining and help with posture and muscle coordination during bowel movements.
Biofeedback Therapy
To improve awareness and coordination of the pelvic floor muscles.



